Monogenic obesity refers to obesity resulting from mutations in a single gene. It is less common than polygenic obesity, which involves variations in multiple genes and is influenced by environmental factors. Monogenic obesity typically manifests early in life and can lead to severe obesity and often, resistance to traditional weight loss methods, including diet and exercise. Here are some examples of genes involved in monogenic obesity:
These genetic mutations are often identified through genetic testing when there is a history of early-onset obesity that does not respond to standard treatment methods. Understanding the genetic underpinnings of obesity can help tailor treatment and management options for affected individuals, including possible hormone replacement therapies (e.g., leptin therapy in leptin-deficient individuals) or targeted medications.
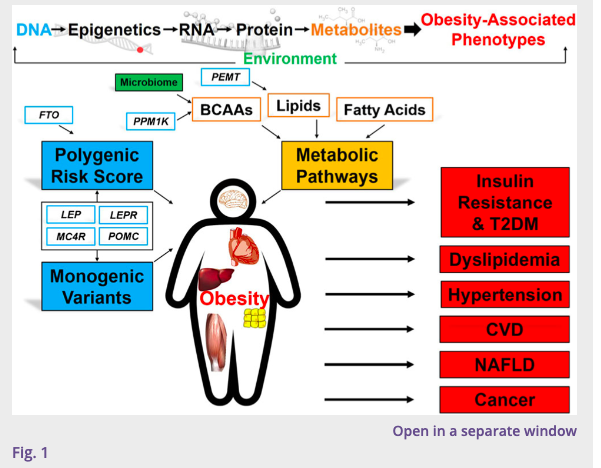
Genomics and metabolic pathways of obesity and associated cardiometabolic risk. Obesity is a systemic disease with impact on the liver, heart, adipose tissue, skeletal muscle, and brain, particularly the hypothalamic-pituitary axis. High-throughput multi-omic profiling (genomic, epigenomic, transcriptomic, proteomic, metabolomic, and microbiome) has advanced the understanding of dysregulated molecular pathways in obesity to improve prediction of cardiometabolic risk. Abbreviations: POMC, pro-opiomelanocortin; LEPR, leptin receptor; LEP, leptin; MC4R, melanocortin 4 receptor; FTO, fat mass and obesity-associated gene; PPM1K, protein phosphatase 1K; PEMT, phosphatidylethanolamine N-methyltransferase; BCAAs, branched-chain amino acids; T2DM, type 2 diabetes mellitus; CVD cardiovascular disease; NAFLD, non-alcoholic fatty liver disease
Connect with Dr. Katakwar and AIG Hospitals:
© 2026 Dr. Abhishek Katakwar. All Rights Reserved.